Safe Delivery: A History of Scottish Midwives
Safe Delivery: A History of Scottish Midwives
 Midwives have performed a vital role for centuries. To help the Royal College of Midwives celebrate the centenary of the Midwives Act (Scotland), 1915, National Records of Scotland presented ‘Safe Delivery: A History of Scottish Midwives’, an archive exhibition telling stories of midwifery before and after professional registration.
Midwives have performed a vital role for centuries. To help the Royal College of Midwives celebrate the centenary of the Midwives Act (Scotland), 1915, National Records of Scotland presented ‘Safe Delivery: A History of Scottish Midwives’, an archive exhibition telling stories of midwifery before and after professional registration.
Midwifery and Scotland
The history of midwifery in Scotland features a number of significant landmarks. In 1726 Joseph Gibson was appointed the world's first Chair of Midwifery by Edinburgh Town Council. William Smellie, a Lanarkshire-born 'man-midwife' who became known as the 'Master of British Obstetrics', published 'A Treatise of the Theory and Practice of Midwifery' in 1752. Sir James Young Simpson, Professor of Midwifery at Edinburgh University, introduced the use of chloroform to relieve labour pains in 1847. It was also in Edinburgh that Dr Elsie Inglis established in 1901 Scotland's first maternity hospital staffed by women. In 1953 Margaret Myles, a midwife and educator from Aberdeen, published the ground-breaking manual 'Textbook for Midwives'. Now in its 15th edition and translated into many languages, 'Textbook for Midwives' is internationally recognised as the essential guide to midwifery.
One book, Thirty-Four years and Two Thousand babies
As long as babies have been born, mothers have had help with the birthing. For centuries the Scottish midwife was called ‘skilly’, ‘handy-woman’, ‘neighbour-woman’, ‘helping-woman’ and, most commonly, a ‘howdie’. A rare birth register records the career of Fife howdie, Margaret Bethune. It is likely that Margaret became a professional midwife to earn a living after her husband William, a coalminer, died in 1852. From 27 February 1853 until a month before her sudden death in 1887, aged 67, she attended 2,034 births throughout the parish of Largo in Fife. They are all contained in one small volume.
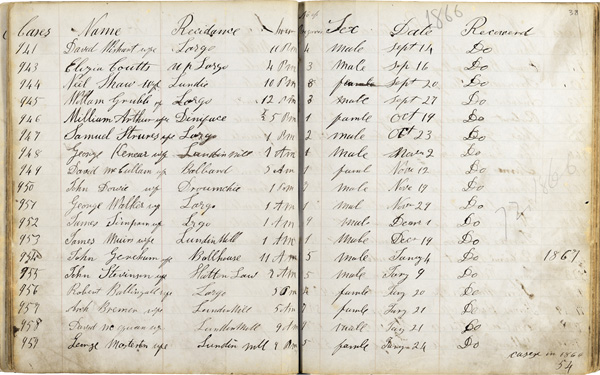
Register of deliveries made by Mrs Margaret Bethune, 1853-1887, p.38
National Records of Scotland, GD1/812/1
Diligently noting the child’s sex, date and hour of birth, and whether the doctor was involved, she also recorded the number of pregnancies for each mother. Margaret’s interest in the babies of her community didn’t end with their births – in some cases she has added the sad details of later deaths such as “died 8 days after of consumption nine months standing”.
The entry for ‘William Arthur wife’ (number 946) relates to the delivery of her own granddaughter, also named Margaret, on 19 October 1866. This was the first child of her daughter and son-in-law. The parents, Margaret and William Arthur later had a son on 24 December 1867, and they named him after his father. This book shows that granny also delivered him into the world.
The Howdies
Before 1915, midwifery was carried out by an assortment of untrained howdies, unregulated nurses and midwives with various degrees of training. Instruction ranged from attending lectures, physician-led courses, learning from another midwife, and teaching in the few maternity hospitals.

Photograph of Mrs McDonald, a midwife in Invercreran, Argyll, c1866
National Records of Scotland, GD1/1208/1/52
‘Lying-In’ hospitals had been established in Edinburgh in 1793 and 1824, and in Glasgow in 1834. In 1879, the oldest of the Edinburgh institutions became the Edinburgh Royal Maternity and Simpson Memorial Hospital funded by a collection to commemorate Sir James Young Simpson’s contribution to obstetrics. Aberdeen General Dispensary, Vaccine and Lying-In Hospital appointed qualified midwives from 1892 and Dundee Royal Infirmary added a maternity ward in 1898. Dr Elsie Inglis established another maternity hospital in Edinburgh in 1901. Some Scottish midwives also trained in England and Ireland.
In 1914 Dr AK Chalmers, Medical Officer of Health for Glasgow, noted that of 380 midwives practising in Glasgow “about 180 have certificates from some teaching school, and nearly 200 are without such” ('The Nursing Times and Journal of Midwifery', 21 February 1914). Mothers were even less likely to have visited maternity hospitals. An estimated 95% of all births at this period - among rich and poor alike – were home births.

Photograph of midwife Elizabeth Sanderson
by kind permission of Dr Iain Hutchison.
Private collection
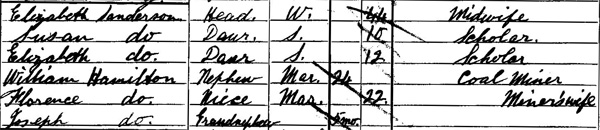
Many midwives took up the job to earn a living after being widowed. Elizabeth Sanderson (1857-1907) married James Sanderson, a coalminer, in 1872 and had given birth to six children by the time he died in 1891. She appears in the 1901 census as a midwife and the head of a household of six, including a 5 month-old granddaughter, in Bothwell, Lanark.
Elizabeth Sanderson, described as 'Midwife' in the 1901 census,
National Records of Scotland, 1901 Census for Bothwell parish, Lanarkshire
Elizabeth Sanderson's daughter remembered:
"From the confinements, she would bring home sheets for the laundering which she did at night. [I remember] as a child often joining [my] mother, at her request in the wash-house to keep her company while she worked there... It was always cold in the wash-house... she was asthmatic and [I believe that] it was the cold, damp conditions of this work that contributed to her death at a relatively early age".
'Midwifery in Scotland: A History' by Lindsay Reid (Scottish History Press, 2011), pp.18-19.
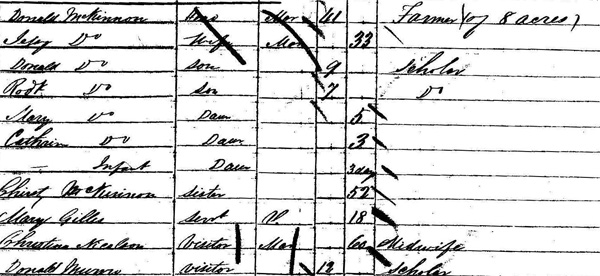
The 1851 census appears to discover one midwife in the process of providing her services to a family on the Isle of Skye. On the night of enumeration, the household of Donald McKinnon, a farmer in Bernisdale in the parish of Snizort, included one infant daughter only 3 days old. The baby had not yet been named at the time of census taking, but would be named Ellen McKinnon. Christina Nicolson, a 60 year old midwife, is also recorded as a visitor to the house. In this period, it was normal practice that midwives would stay with the mother and their new baby for several days after the birth and was especially so in remote areas where transport might be difficult. By the 1861 census, the McKinnon family had grown to include seven children; Donald, Robert, Mary, Catherine, Ellen, Charles and Flora.
Christina Nicolson described as 'Midwife' in the 1851 census,
National Records of Scotland, 1851 Census for Snizort parish, Skye
Before the Central Midwives Board it is difficult to assess the number of midwives practising in Scotland as they don’t often feature in official records. The 1911 census records only 313 midwives whereas a total of 3,161 midwives were registered in the first two years of the Board coming into being.

Photograph of Edinburgh-born midwife,
Isabella Charles with her sister.
Private collection
A matter of life and death
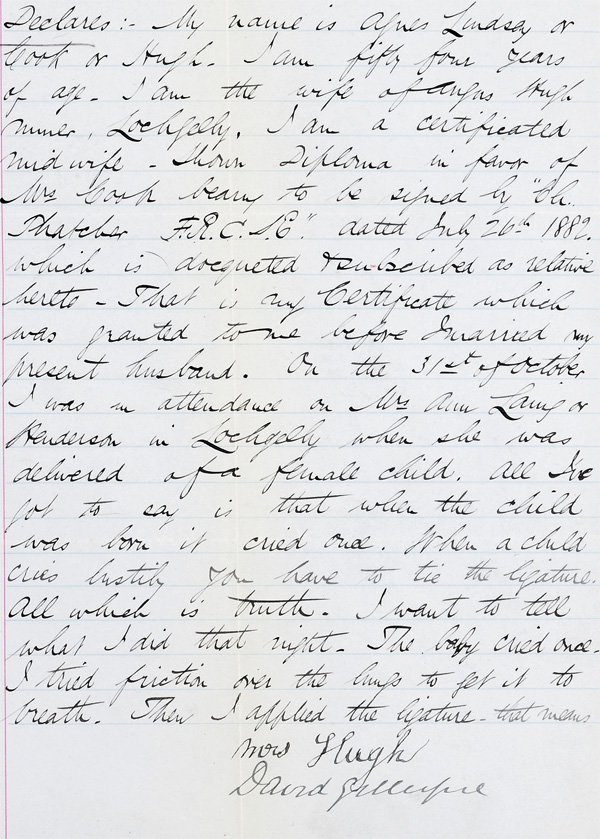
An 1888 criminal trial reveals the dangers of unregulated midwifery. Agnes Hugh, a certificated midwife working in Fife was accused of the crime of culpable homicide caused by her failure to tie the umbilical cord following the birth of a girl to Ann Laing and Archibald Henderson on 31 October 1887 at Well Road, Lochgelly.
Agnes Hugh's Declaration, trial papers
relating to the crime of culpable homicide , 1888
National Records of Scotland, JC26/1888/1
Transcription of Agnes Hugh's Declaration, National Records of Scotland, JC26/1888/1 (pdf)
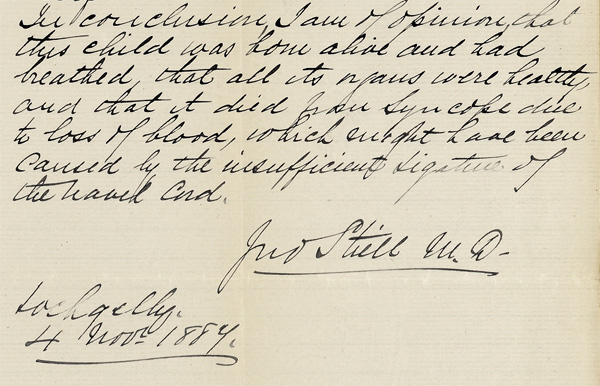
The medical report by Dr John Stiell’s states that “The body was that of a fairly well nourished female child born at the full term of uterine gestation… [and] it died from loss of blood which might have been caused by the inefficient ligature of the navel cord”.
Various relatives and neighbours gave evidence at the trial. Isabella Henderson went to the house of her sister-in-law and “found her in bed suffering from labour pains… The midwife was standing at Annie’s bedside attending to her in some way… I saw at once that the midwife was under the influence of drink” and later “it was evident that she had been having more drink – she was very bad she could hardly stand”. After the birth she saw “ that blood was coming freely from the child’s navel and that no attempt had been made to tie the cord”. The father declared that “When I left there was a quart bottle of whisky in the house – it was not quite full… my sister came outside and told me that the baby which had been born alive was dead… I looked at the whisky bottle and found it was empty”.
The declarations also reveal that Agnes Hugh became angry at the suggestion of working with a doctor. When a neighbour Helen Donnachie, sent for Dr Stiell “The woman still did nothing and continued scolding me and saying what did she care for the Doctor and that her education was paid for and a lot of drunken nonsense, during which time the child died [and]… left but not before abusing everyone in the house and demanding to be paid 7/6 there and then.” (National Records of Scotland, JC26/1888/1).
Agnes Hugh denied the accusation but was convicted of the crime and sentenced to 12 months imprisonment.
Dr John Stiell's Declaration from papers relating to the trial
of Agnes Hugh for culpable homicide, 1888
National Records of Scotland, JC26/1888/1
Not all midwives shared Agnes Hugh’s attitude towards doctors. Mima Sutherland, a midwife working in Unst, Shetland, during the Second World War, recalled:
“I attended the births myself very often but if I was worried about anything Dr Saxby would come with me. When we were together he would deliver the baby – you see he was a marvellous obstetrician – oh he was gifted. I would act as his assistant. He was renowned… Most times I went by myself. The mothers had everything ready. They would get in the wool. We used to get a reel of special ties for the umbilical cord. My dad called me a peerie howdie. When I returned from a case he would be walking up and down and all he would say was ‘Is the woman all right? And I would say, ‘Yes, she’s fine’…”
'Scottish Midwives Twentieth Century Voices' by Lindsay Reid (Tuckwell Press, 2000), pp.20-21.
‘Practically without any one possessed of medical skill’
Although the nineteenth century saw developments in welfare provision, midwifery services were not included, leaving some communities poorly-provided. In 1899 the residents of North Ronaldsay, Orkney, were in desperate need of a midwife. A letter from William Muir to the Congested Boards District recounts their plight:“The population is 501, there are two churches and one school, they have two midwives, one is over 80 and the other is over 90 years of age, they are practically without any one possessed of medical skill or even of nursing in cases of sickness” .
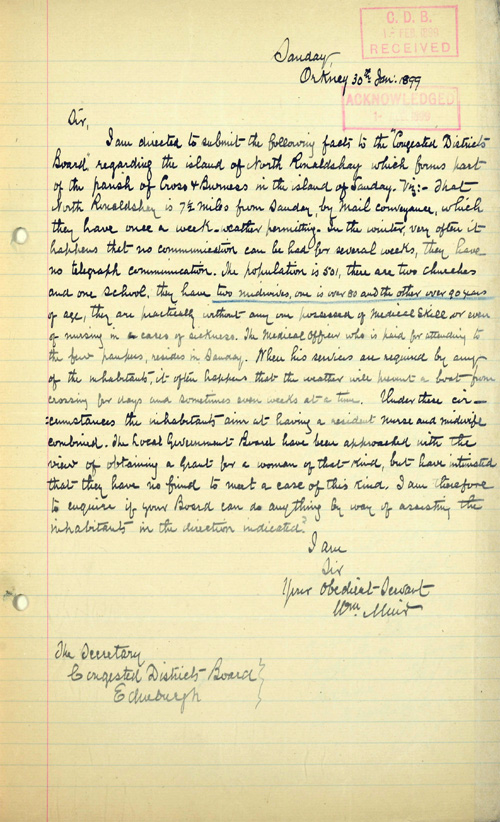
Application to the Congested Districts Board for a nurse-midwife, 1899
National Records of Scotland, AF41/323/4
The younger of these elderly midwives was Sarah Swanney, widow of Thomas Swanney. She died on 20 January 1912 at the age of 92. The elder, Mary Muir, widow of John Muir, a weaver, died on 31 January 1905 at the age of 95. Given the difficulties of sailing to the small island in extreme weather and the age of the retired midwives, the community felt that a resident nurse-midwife was necessary and sought help from the government.
The Local Government Board which was responsible for public health refused to help as it had no fund for midwives. Next, the islanders turned to the recently constituted Congested Districts Board. This Board’s function was to aid the Highlands and Islands with agricultural equipment, lighthouses, piers, harbours and bridges – but unfortunately not nurses or midwives. It was suggested that the islanders turn to the Queen Victoria Jubilee Institute for Nurses instead.
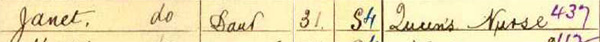
This charity was created by the Queen in 1887 by a donation of £70,000 from the Women’s Jubilee Fund to provide training, support, maintenance and supply of nurses for the sick poor. The inhabitants of North Ronaldsay found a solution here. The 1901 census records that Helen Nobel, a 29 year old ‘Queen’s Nurse’ born in England, was lodging at the Tulloch family croft on the island. She seems to have left an impression. Ten years later, Janet Tulloch, now 31, had become North Ronaldsay’s home-grown ‘Queen’s Nurse’.
Janet Tulloch described as 'Queen's Nurse' in the 1911 Census for North Ronaldsay
‘A situation of grave urgency’
The Midwives Act, 1902, created a Central Midwives Board to regulate the profession in England and Wales. During parliamentary debates MPs noted that Britain was the only civilised country in Europe without some sort of midwifery registration and regulation. However the number of provisions and amendments required to bring the Act into Scottish law were thought too complex so Scotland was not included, despite growing concerns for child health north of the border.
The outbreak of war in August 1914 brought pressure from an unexpected direction. A year later the Scottish medical profession addressed this memorial to the authorities calling for a Midwives Act for Scotland. They felt that the need for such was “already great, independently of the present war conditions” but had now become “a situation of grave urgency” (Memorial of the Medical Faculties of the Universities, the Royal Medical Corporations and the Medical Officers of the Maternity Hospitals in Scotland to HM Secretrary for Scotland and the Lord President of HM Privy Council anent a Midwives Bill for Scotland, 1915, National Records of Scotland, CMB4/2/8).
In 1906, the First National Conference on Infant Mortality was held in London, reflecting the growing Infant Welfare Movement and leading to the 1907 Notification of Births Act. This law required notification within 36 hours to the Medical Officers of Health, the local authority officials responsible for public health, a practice which drew their attention to the inconsistent nature of midwifery. Adopted by the main cities in Scotland from the outset, legislation made this practice compulsory in 1915.
At the 1914 Nursing Conference, influential Medical Officer of Health for Glasgow, Dr AK Chalmers, argued for a Midwives Act for Scotland. He proposed the resolution that “this meeting of nurses and others interested in nursing and the welfare of mothers and infants unanimously and earnestly urge upon the Secretary for Scotland the great need for an Act for the protection of women in child-bed, and for the training and supervision of women practising as midwives in Scotland” ('The Nursing Times and Journal of Midwifery', 21 February 1914).
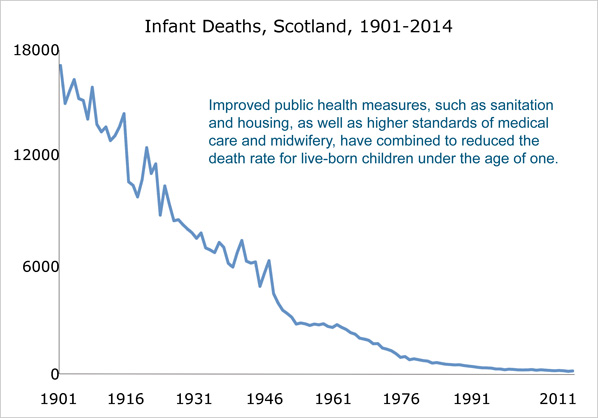
We hereby certify…
In 1916 the Central Midwives Board for Scotland took control of the midwifery profession. From 1 May the Board recorded certificated midwives in registers detailing their names, addresses, date of enrolment and qualifications. During the first two years midwives were eligible if they had been in bona fide practice since 1914 and were "trustworthy, sober and of good character". They became known as ‘'bona fides’. A total of 1,569 midwives were registered in 1916 and another 1,592 the following year.
This 1916 Order by the Privy Council of King George V brought the Central
Midwives Board for Scotland into being and approved the first set of Rules.
National Records of Scotland, CMB4/2/8
The first Midwives Roll for Scotland, 1916-1920
National Records of Scotland, CMB5/1
Qualifications were accepted from the Scottish maternity hospitals as well as institutions in Dublin and London, as were certificates issued by the Central Midwives Board for England and Wales. The earliest qualifications included were those of Glaswegian Margaret Duncan, who trained at Coombe Lying-In Hospital, Dublin in 1866, and Elizabeth McDonald who had qualified at the Royal Maternity Hospital in Edinburgh in 1876. Other ‘bona fides’ may have been practising for just as long but the register only notes ‘In practice December 1914’ as this was the date that mattered.
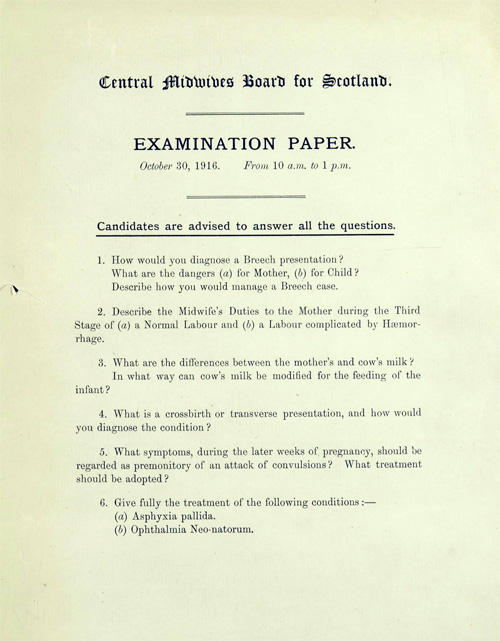
First Central Midwives Board for Scotland examination paper, 30 October 1916,
National Records of Scotland, CMB4/5/1
The first exam was held on 30 October 1916. At the 1917 Maternity and Child Welfare Conference the Board’s Chairman Sir John Halliday was pleased to note that around one third of these 77 candidates were ‘bona fides’ who elected to gain admittance to the roll by passing the examination even though they didn’t have to. Around 300-400 professionals qualified by examination annually from 1918.

Paisley midwife Elizabeth Campbell Muldoon
and her son Willy, private collection.

Entry for Elizabeth Muldoon in the first Midwives Roll for Scotland
National Records of Scotland, CMB5/1, page 182
Second World War
By 1939 the majority of midwives were also trained nurses and joined up for active service during the Second World War. The government anticipated the impact upon midwifery in Britain and instituted a voluntary version of National Service whereby midwives committed themselves to the role for the duration of the war. In 1943, the Midwives (Registration for Employment) Order made it compulsory for all State Certified Midwives, whether practising or not, and any pupil midwives, to register with the Employment Exchange on 10 April 1943.
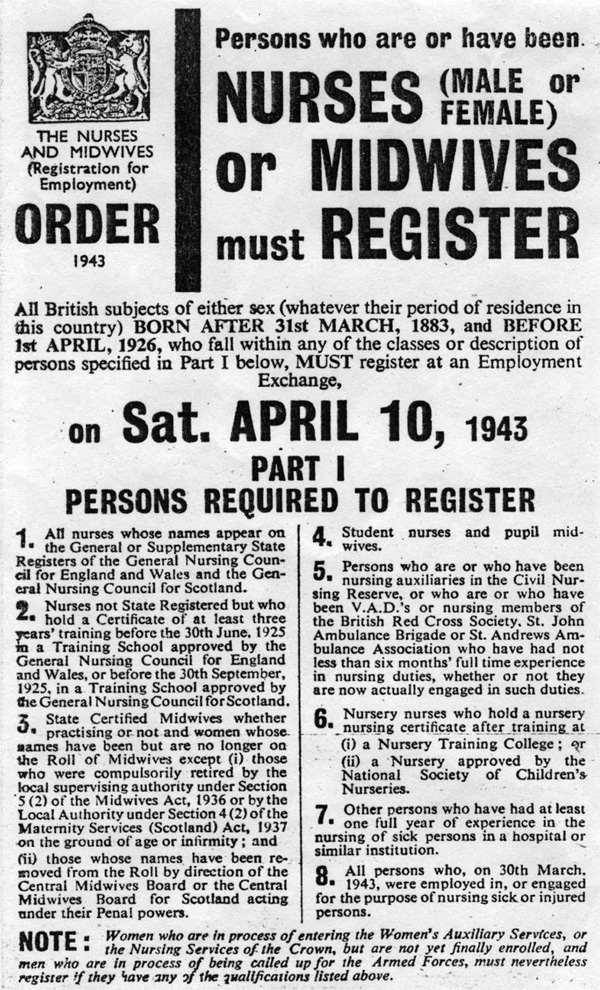
1943 Nurses and Midwives (Registration of Employment) Order
issued by the Ministry of Labour and National Service.
Private collection
The Second World War brought other challenges to midwives and mothers. Many pregnant women were evacuated to emergency maternity hospitals in converted country seats such as Airthrey Castle, Stirlingshire, but many others gave birth at home under difficult conditions.
Alice Porter was a pupil midwife in Aberdeen in the 1940s:
“The windows had been blown out and the stairways were blown out and had no bannisters… I could not leave the young woman so I asked the policeman to come back in a couple of hours... Just before the child was born the sirens sounded and the blast blew out the sacking covering the windows and soot blew into the room from the roofs. Under these conditions I delivered the baby. The policeman arrived with an ambulance. I carried the new baby down the broken stairway to the waiting ambulance and mother and child were transported to hospital.”
Mima Sutherland was a midwife on Unst, Shetland, during the Second World War:
[The RAF station] “had some narrow escapes. When this mother was in labour, doctor and I had to wait at the gate because there was an air-raid warning... She was very brave. She made supper and then as soon as supper was by she… went to her room and the baby was born almost immediately.”
Passages from 'Midwifery in Scotland: A History' by Lindsay Reid, p.101.
'Shades approved by the Board'
Professional regulation extended to the way that midwives dressed. Distinctive uniforms were introduced by the Central Midwives Board for Scotland, the Queen’s Nursing Institute and other institutions. Glasgow Corporation midwives were known as ‘Green Ladies’ because of theirs.
In 1948 the Central Midwives Board for Scotland issued a booklet and application form detailing the approved uniform. The precisely specified garments were many; overcoat, lightweight overcoat, raincoat, jacket, skirt, blouse, tie, cloak, headwear, dress, indoor cap, buttons, badges, gloves, shoes and stockings. The colours were predominantly mid grey and blue with black shoes and had to conform “strictly to the shades approved by the Board" (National Records of Scotland, CMB4/3/17).
State certified midwives could only purchase the uniform from an approved list of tailors with their certificate number and a permit from the Board. Official badges were embroidered on the hat, cap or beret and for the dress metal brooches – capable of withstanding disinfection – could be obtained with a postal order for 6 shillings. The midwife was also instructed to take care that her uniform and badge “do not fall into the hands of unauthorised persons”.

Queen's Institute District Nurses were trained in both
nursing and midwifery and wore blue uniforms.
Photograph by William Elsmore, private collection.
Call the Midwife
After the war the National Health Service (NHS) came into being, providing free health services for all from 1948, funded by central government, local rates and a public national insurance scheme. The NHS did not affect the operation of the Central Midwives Board but fragmented the provision of midwifery services. General Practitioners became the first point of contact for pregnant women and performed increasing amounts of antenatal care, Hospital births became more common and certified midwives continued to attend home births, often travelling by bicycle.
Midwife Margaret Dearnley trained in Glasgow during the 1940s:
"Now the poverty was dreadful. Very, very bad. I remember going in a house which was all dark, but a great big roaring fire. And there were two or three kids running about… with wee vests on and nothing else and a packed earth floor. And the new mother… was lying on what they call ticking on a bed, an iron bedstead in the corner.”
'Midwifery in Scotland: A History' by Lindsay Reid, p.177.
Midwife Anne Bayne qualified at Aberdeen Royal Infirmary in 1951:
“I had a break and came back into midwifery in 1964… I used to tell the students that home confinements went oot o the window when interior spring mattresses and fitted carpets came in. At that time if you bought one it was for a lifetime”.
Ella Cleland qualified in Glasgow in 1958:
“There was a lot of poverty in Glasgow and they gave us money to give to the husband to phone… One time a husband was sent with a quick message to say that his wife was ‘fully dilated’ and he told sister that his wife was ‘fully delighted’.”
Passages from 'Scottish Midwives: Twentieth Century Voices' by Lindsay Reid, p.108, p.117.
The Royal College of Midwives
The Royal College of Midwives originated in London in 1881 when Zepherina Veitch, a nurse who had served in the Franco-Prussian war, established the Trained Midwives Registration Society. The aims were to improve midwifery training and to campaign for the government to regulate the profession. The name was soon changed to the Midwives Institute.
By 1901 the Institute had created an insurance scheme for midwives who required legal defence, needed to pay doctors fees, or were unable to work because of puerperal fever quarantine. The Midwives Institute also maintained an employment register and continued to provide education in midwifery and campaign for legislation. In 1941 it changed its name to the College of Midwives and in 1947 received a Royal Charter.
The Scottish Midwives’ Association was inaugurated by Mrs Quentin Smith in 1917 and in 1946 voted to join the College, becoming the Scottish Council of the Royal College of Midwives. Today, the RCM represents the interests of midwives in all parts of the UK and promotes excellence, innovation and leadership in the care of childbearing women, the newborn and their families.
The functions of the Central Midwives Board for Scotland (collection reference CMB), together with the General Nursing Council for Scotland (collection reference GNC), were taken over by a new National Board for Nursing, Midwifery and Health Visiting for Scotland (collection reference NMH) in 1983. For information about the archives of other Scottish public bodies see our records guide on Scottish Government Records after 1707. You can search these collections in the National Records of Scotland online catalogue.
Further Reading: Lindsay Reid 'Scottish Midwives: Twentieth Century Voices' (Tuckwell Press, 2000), republished (Black Devon Books, 2008); and 'Midwifery in Scotland: A History' (Scottish History Press, 2011).
![Privy Council Order [expand], National Records of Scotland, CMB4/2/8](/files//research/MidwivesFeatureRulesCMB4-2-8-1.jpg)
![The Midwives Roll for Scotland, [dates], p.99, National Records of Scotland, CMB5/1](/files//research/MidwivesFeatureRegisterCMB5-1-p99.jpg)